- HEALTHY GUT HEALTHY THYROID
- Posts
- 3 Types of Immune Tolerance, Short Chain Fatty Acids
3 Types of Immune Tolerance, Short Chain Fatty Acids
Healthy Gut Healthy Thyroid Newsletter!

Welcome to Healthy Gut Healthy Thyroid!
This is your weekly roundup of the BEST actionable steps for those people with thyroid and autoimmune thyroid conditions who want to restore their health…by healing their gut. Whether you have hyperthyroidism or Hashimoto’s you will benefit from the content in this newsletter.
In today's issue:
Main Topic: The Relationship Between Immune Tolerance, the Gut Microbiome, and Thyroid Autoimmunity
Podcast Review: 7 Gut Healing Roadblocks That Can Stall Thyroid Recovery
Understand Your Tests: Understanding Short Chain Fatty Acids
Ask Dr. Eric: What are the consequences of low dietary fiber?

The Relationship Between Immune Tolerance, the Gut Microbiome, and Thyroid Autoimmunity
Most people have heard of the immune system—but fewer are familiar with the concept of immune tolerance. Simply put, immune tolerance is the body’s ability to recognize what is safe and what is not, and to respond appropriately. When this system breaks down, the immune system can mistakenly attack food proteins, chemicals, or even the body’s own tissues.
A loss of immune tolerance is a key driver in the development of autoimmune conditions such as Graves’ disease and Hashimoto’s thyroiditis. Understanding the role of the gut microbiome in maintaining immune tolerance is essential for reversing or preventing thyroid autoimmunity.
Much of what I’ve learned about immune tolerance has come from the work of Dr. Datis Kharrazian. One of the key concepts from his work is that there are three types of immune tolerance, each of which can be compromised in different ways.
The Three Types of Immune Tolerance
Oral Tolerance. This refers to the immune system’s ability to tolerate food proteins. When this type of tolerance is lost, the immune system may overreact to harmless foods, resulting in food sensitivities, bloating, gas, and inflammation.
Chemical Tolerance. This is the tolerance to environmental chemicals such as mold toxins, pesticides, and solvents. People with multiple chemical sensitivity (MCS) often have a loss of chemical tolerance. Testing options, such as Cyrex Labs Array #11, can help identify this.
Self Tolerance. This refers to the body’s ability to tolerate its own tissues. When self-tolerance is lost, the immune system begins attacking the body’s organs or tissues. In Graves’ disease, the immune system targets TSH receptors. In Hashimoto’s, it targets thyroglobulin and thyroid peroxidase, which can be confirmed through antibody testing.
What Are Antigens, and Why Do They Matter?
An antigen is any substance that triggers an immune response. Antigens can include:
Undigested food proteins
Environmental chemicals
Pathogens
Tissue from your own body (in autoimmune conditions)
In thyroid autoimmunity, proteins within the thyroid gland are mistakenly recognized as antigens. The immune system attacks these tissues, causing inflammation and dysfunction.
Proper digestion plays a critical role in minimizing antigenic load. When food isn’t fully broken down—due to low stomach acid, reduced bile production, or insufficient digestive enzymes—larger, partially digested molecules may enter the gut and provoke an immune response.
Mindful eating and thorough chewing are often overlooked but powerful strategies. Taking time to chew your food well helps initiate digestion and can lower the burden on the gut and immune system.
Secretory IgA: The First Line of Mucosal Defense
Secretory IgA (SIgA) is a protective immune protein found in the mucous membranes of the gut, respiratory tract, and other mucosal tissues. It plays a vital role in regulating immune tolerance by helping the immune system distinguish between friend and foe.
Low SIgA levels are commonly found in individuals with chronic stress, leaky gut, or gut infections, and may indicate a reduced ability to tolerate food and environmental antigens. While low SIgA doesn’t confirm a leaky gut, it is often associated with increased intestinal permeability.
The Role of Dendritic and Kupffer Cells in Autoimmunity
Dendritic cells are like security guards of the immune system. They present antigens to other immune cells and help determine whether to mount an immune response. When the body is in a pro-inflammatory state, dendritic cells can become overactive, increasing the risk of autoimmunity.
Kupffer cells are immune cells in the liver that process microbial and dietary antigens that enter through the gut. If someone has gut dysbiosis or a leaky gut, these cells can become chronically activated, producing inflammatory cytokines and oxidative stress—both of which can contribute to thyroid autoimmunity.
Interestingly, hyperthyroidism may enhance Kupffer cell activity, further increasing oxidative stress.1
Regulatory T Cells (Tregs) and Immune Balance
Regulatory T cells (Tregs) are essential for maintaining immune tolerance. They act like peacekeepers, calming the immune response and preventing it from attacking your own tissues. A deficiency in Tregs is linked to autoimmune diseases, including Graves' and Hashimoto’s.
To support Treg activity:
✅Maintain healthy vitamin D levels – Vitamin D helps increase Treg populations and suppresses autoimmune responses. Aim for serum levels between 50–70 ng/mL, ideally under practitioner guidance.
✅Exercise regularly – Moderate physical activity has been shown to boost Treg function.
✅Sleep and stress management – Chronic stress and poor sleep reduce Treg activity, while restorative sleep and relaxation techniques can enhance it.
A Diverse Gut Microbiome Supports Immune Tolerance
A diverse gut microbiome plays a major role in shaping immune responses. Low microbial diversity is associated with inflammation, immune dysregulation, and autoimmunity.
To increase microbiome diversity:
➡️Eat a wide range of plant-based foods: Strive for 40+ different plants per week, including fruits, vegetables, herbs, spices, whole grains, and legumes.
➡️Include resistant starches: Found in green bananas, cooked and cooled potatoes, and legumes, resistant starch feeds beneficial bacteria.
➡️Enjoy fermented foods: Such as sauerkraut, kefir, coconut yogurt, and kimchi (if tolerated).
➡️Rotate your foods: Don’t eat the same meals every day—variety feeds different bacterial species.
Avoid or minimize:
✔️Antibiotics (unless absolutely necessary)
✔️Proton pump inhibitors (PPIs)
✔️Glyphosate-containing foods
✔️Chronic use of medications that disrupt gut flora (e.g., NSAIDs, antithyroid meds)
The Role of Short-Chain Fatty Acids (SCFAs)
SCFAs—especially butyrate, acetate, and propionate—are produced when gut bacteria ferment dietary fiber. These compounds:
✔️Strengthen the gut barrier
✔️Nourish colon cells
✔️Reduce inflammation
✔️Stimulate Treg development
Butyrate is the most studied SCFA and is especially important for intestinal integrity and immune modulation. You can increase SCFA production by eating:
➤Fruits: Apples, berries, bananas
➤Vegetables: Onions, asparagus, Jerusalem artichokes
➤Legumes: Lentils, black beans, jelly beans
➤Nuts & seeds: Pistachios, flaxseeds
If you experience bloating with high-fiber foods, consider a butyrate supplement as a postbiotic alternative.
Nutrients That Support Immune Tolerance
Certain nutrients play an essential role in immune regulation and tolerance:
➤Vitamin D – Promotes Treg activity and reduces autoimmune reactivity
➤Omega-3 fatty acids (EPA/DHA) – Reduce inflammation and promote immune balance
➤Glutamine – Repairs the gut lining and supports SIgA production
➤Zinc – Critical for T cell function and gut barrier integrity
➤Selenium – Antioxidant that reduces oxidative stress in autoimmune thyroid disease
➤Magnesium – Regulates inflammation and supports immune modulation
➤Polyphenols – Found in berries, green tea, turmeric, and olive oil; support microbial diversity and reduce oxidative stress
Conclusion
Immune tolerance is the foundation of a balanced immune system, and its loss is central to the development of autoimmune thyroid conditions like Graves' disease and Hashimoto’s. The gut microbiome plays a key role in maintaining this tolerance by regulating antigen exposure, supporting regulatory T cells, and producing anti-inflammatory compounds like short-chain fatty acids.
Through a combination of nutritional strategies, gut healing protocols, and lifestyle modifications, you can begin to restore immune tolerance and reduce autoimmune reactivity. Whether you're managing a current thyroid condition or working to prevent one, supporting your gut is not just helpful—it’s essential.

Which Hyperthyroid Healing Diet Should You Follow?
There’s no single diet that everyone with hyperthyroidism should follow. Diet selection is a highly personal choice that must consider individual health conditions, lifestyle, and preferences.
In my book, The Hyperthyroid Healing Diet, I explore three different diets in detail, explaining what each involves and how you can start implementing the right one for you. This book will benefit those with Graves' disease, toxic multinodular goiter, and subclinical hyperthyroidism.
There is a lot of confusion when it comes to the foods people with hyperthyroidism should eat and which ones they should avoid, and the truth is that there isn’t a single diet that fits everyone perfectly. That’s why The Hyperthyroid Healing Diet doesn’t just focus on one diet, but instead gives multiple diet options, while at the same time guiding you towards the one most suitable for your situation and condition.
Note: those who purchase The Hyperthyroid Healing Diet will also gain access to the online resources, which includes dozens of recipes, checklists related to the different diet options, and a few bonus chapters not included in the book.
By reading this book you will discover the following:
✅ The ideal diet for Graves’ disease, toxic multinodular goiter, subacute thyroiditis, and subclinical hyperthyroidism
✅ Hidden sources of common allergens and other ingredients to avoid 3 ways to detect specific food triggers
✅ How much protein those with hyperthyroidism should consume on a daily basis
✅ The truth about food sources of iodine
✅ How to increase muscle mass and bone density
✅ What diet you should follow if you’re a vegan or vegetarian
✅ Addressing weight loss and weight gain concerns
✅ What you need to do to achieve optimal adrenal health How to optimize your adrenals, improve sleep quality and duration, and heal your gut
✅ And much, much more!
Click Here to Order the Hyperthyroid Healing Diet

Save My Thyroid Podcast Review
I have a podcast called "Save My Thyroid", where I discuss how people with hyperthyroidism and Hashimoto's can save their thyroid and regain their health. And during each edition of this newsletter I'll briefly discuss a recent podcast episode.
In a recent podcast episode I discussed “7 Gut Healing Roadblocks that Can Stall Thyroid Recovery” In this episode, we take a closer look at seven common gut-related roadblocks that can interfere with thyroid healing. That includes foods like gluten, grains, and nightshades but also deeper layers like low stomach acid, gut infections, and hidden stress. You’ll also hear about environmental factors such as glyphosate and xenoestrogens that can negatively affect gut integrity over time.
Overall, it’s about understanding what could be getting in the way, and making thoughtful shifts where it makes sense. Healing the gut is often a foundational step, especially for autoimmune thyroid conditions.

Understand Your Tests
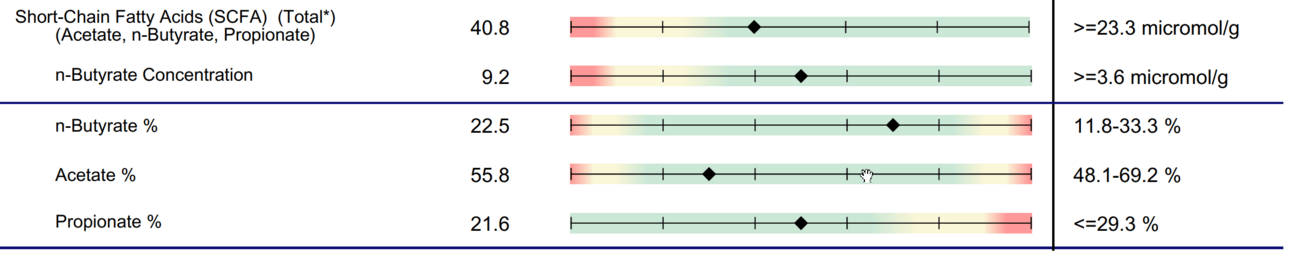
Patient Test #1: Normal SCFAs
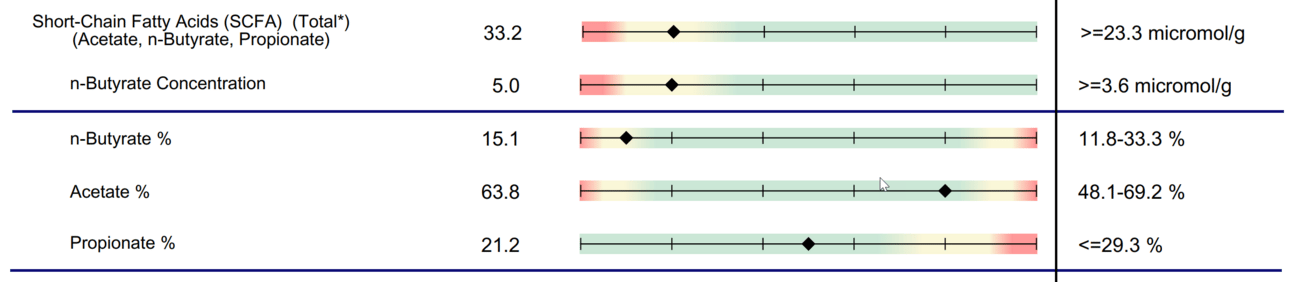
Patient Test #2: Total SCFAs low
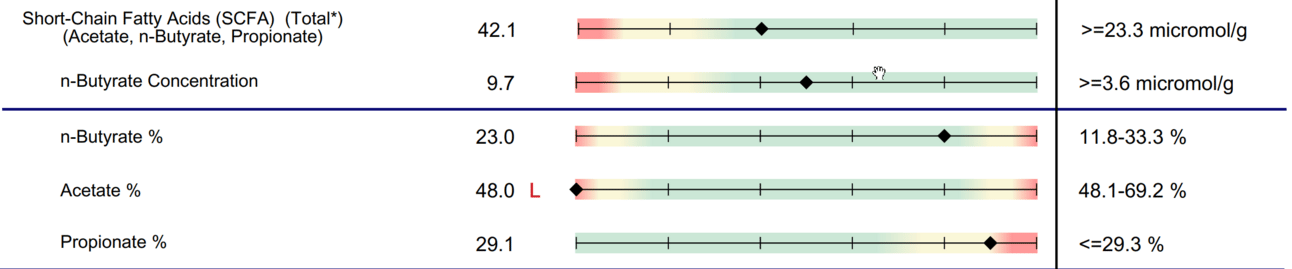
Patient Test #3: Low Acetate %
Understanding Short Chain Fatty Acids
While I don’t routinely test all patients for short-chain fatty acids (SCFAs), this topic is important enough to address—especially for those dealing with gut imbalances and thyroid autoimmunity. SCFAs are metabolic byproducts produced when gut bacteria ferment dietary fiber, and they play a key role in maintaining gut and immune health.
When I order a comprehensive stool analysis, I typically use the GI-MAP, which unfortunately does not measure SCFAs. However, other functional stool tests—such as the GI Effects from Genova Diagnostics—do measure these markers.
Regardless of whether SCFAs are tested, I almost always recommend that patients increase their intake of fiber-rich and resistant starch foods. However, if testing reveals low levels of butyrate, it may also be beneficial to consider supplementing with a butyrate supplement as part of a broader gut healing protocol.
Patient Case Examples
Patient Test #1 – Normal SCFAs This patient’s test shows a healthy SCFA profile:
n-Butyrate concentration is within the optimal range
Acetate and propionate percentages are also balanced
This is exactly what we want to see: well-balanced SCFA production that reflects healthy microbial fermentation of fiber.
Patient Test #2 – Low SCFAs
Here, the total SCFA level is low. The primary issue is a low n-butyrate concentration and percentage, while acetate and propionate are within normal limits. This suggests that fiber is being consumed, but the microbial activity needed to produce butyrate may be insufficient.
In such cases, the focus should be on:
Increasing fiber intake (especially resistant starches)
Supporting microbial diversity
Possibly supplementing with butyrate or butyrate precursors
Patient Test #3 – Low Acetate %
This test reveals normal total SCFAs, with n-butyrate and propionate in range, but a low acetate percentage. While butyrate gets a lot of attention, acetate is also important—it serves as a substrate for energy production and supports cross-feeding between bacterial species.
In this scenario, boosting overall dietary fiber intake remains the top recommendation.
In the “Ask Dr. Eric” section below I’ll discuss some of the consequences of having low levels of SCFAs.

Ask Dr. Eric

During every issue I'll answer a question or two that I think can benefit most people with a thyroid or autoimmune thyroid condition. If you'd like for me to consider your question for a future edition of this newsletter email your question to [email protected].
QUESTION: WHAT ARE THE CONSEQUENCES OF LOW DIETARY FIBER?
Dr. Eric, I’ve heard that a carnivore diet can benefit those with autoimmune conditions, but I’ve also heard that restricting fiber for a prolonged period of time can be a concern, and wanted to know your thoughts.
Thank you for your question! There are numerous health benefits of dietary fiber, and one of the main benefits is that it’s essential for the production of short chain fatty acids (SCFAs), which I discussed in the “Understand Your Tests” section.
Having sufficient dietary fiber is important for a healthy gut microbiome, and a big part of this relates to having adequate levels of SCFAs. In other words, if you don’t consume enough dietary fiber you probably will have low levels of SCFAs.
Low levels of SCFAs—particularly butyrate, acetate, and propionate—can have wide-ranging consequences for gut and overall health. Here’s how SCFA deficiency can affect the body:
✅Compromised Gut Barrier Integrity. Butyrate is essential for maintaining the intestinal epithelial barrier. It fuels colonocytes (gut lining cells) and promotes tight junction integrity. Low butyrate levels are associated with:
Leaky gut
Increased risk of autoimmune activation
Greater exposure to inflammatory antigens and pathogens
✅Increased Inflammation. SCFAs have strong anti-inflammatory properties, both in the gut and systemically. They modulate immune responses by:
Promoting Treg development, which helps prevent autoimmune activity
Inhibiting pro-inflammatory cytokine production
Without adequate SCFAs, there’s an increased risk of chronic low-grade inflammation, which can drive weight gain, fatigue, and thyroid dysfunction.
✅Altered Immune Function. Low SCFAs—especially butyrate—can impair immune regulation. This may result in:
Increased susceptibility to infections
Reduced oral tolerance to food proteins
Greater likelihood of immune dysregulation and autoimmunity, including Graves’ disease and Hashimoto’s thyroiditis
✅Blood Sugar Dysregulation and Insulin Resistance. SCFAs help to regulate glucose homeostasis by:
Enhancing insulin sensitivity
Supporting GLP-1 and PYY secretion (gut hormones that regulate appetite and blood sugar)
Low SCFA levels may contribute to insulin resistance, sugar cravings, and weight gain—especially in thyroid patients with slowed metabolism.
✅Impaired Nutrient Absorption. SCFAs help maintain proper gut motility and nutrient absorption. A deficiency can contribute to:
Bloating, constipation, or diarrhea
Malabsorption of essential nutrients, including vitamins and minerals required for thyroid health (e.g., selenium, zinc, magnesium)
✅Disrupted Gut-Brain Communication. Butyrate plays a role in the gut-brain axis by modulating neurotransmitter production and reducing neuroinflammation. Low levels may be associated with:
Brain fog
Anxiety and mood disturbances
Impaired vagus nerve signaling
How to Support SCFA Production Naturally
To restore SCFA levels and promote gut health:
Eat a wide variety of fiber-rich plant foods (aim for 40+ per week)
Include resistant starches: green bananas, cooked & cooled potatoes, legumes
Add fermented foods like sauerkraut, coconut yogurt, or kimchi (if tolerated)
Consider a butyrate supplement if digestive symptoms limit fiber intake
Avoid unnecessary use of antibiotics, NSAIDs, and other gut-disrupting medications
Manage stress to support vagal tone and digestive motility

Additional Thyroid-Related Resources
Click Here for 7 Gut Healing Roadblocks That Can Stall Thyroid Recovery (episode 205)
Click Here for What Thyroid Sufferers Need To Know About Fiber, Resistant Starch, and SCFA (article)
Click Here to access hundreds of thyroid-related articles and blog posts
Click Here to join the Graves’ disease and Hashimoto’s community
Click Here to purchase one of Dr. Eric’s thyroid-related books
Click Here to work with Dr. Eric and his team
📚References:

I hope you enjoyed this week’s newsletter!
Dr. Eric
P.S. This newsletter is a work in progress. I'm writing this newsletter for you, and so please reply and tell me what you liked or disliked about it and what else you'd like to see (or click one of the buttons below)
What did you think of this week's edition?Tap below to let me know. |